05/25/2023
Medical coding forms the backbone of healthcare billing, enabling smooth claims processing, accurate reimbursements, and comprehensive patient records. As healthcare rapidly evolves with policy shifts, technological innovations, and emerging patient care standards, medical coding must adapt to meet these changes. By 2025, this critical field will experience significant transformation driven by advancements like artificial intelligence, automation, and the expansion of telehealth services.
Coders will also play an essential role in value-based care models, mental health and chronic disease management, and navigating complex regulatory updates. These changes highlight the growing importance of medical coders in ensuring efficient healthcare operations and financial accuracy.
Let’s delve into eight predictions that will shape the future of medical coding by 2025.
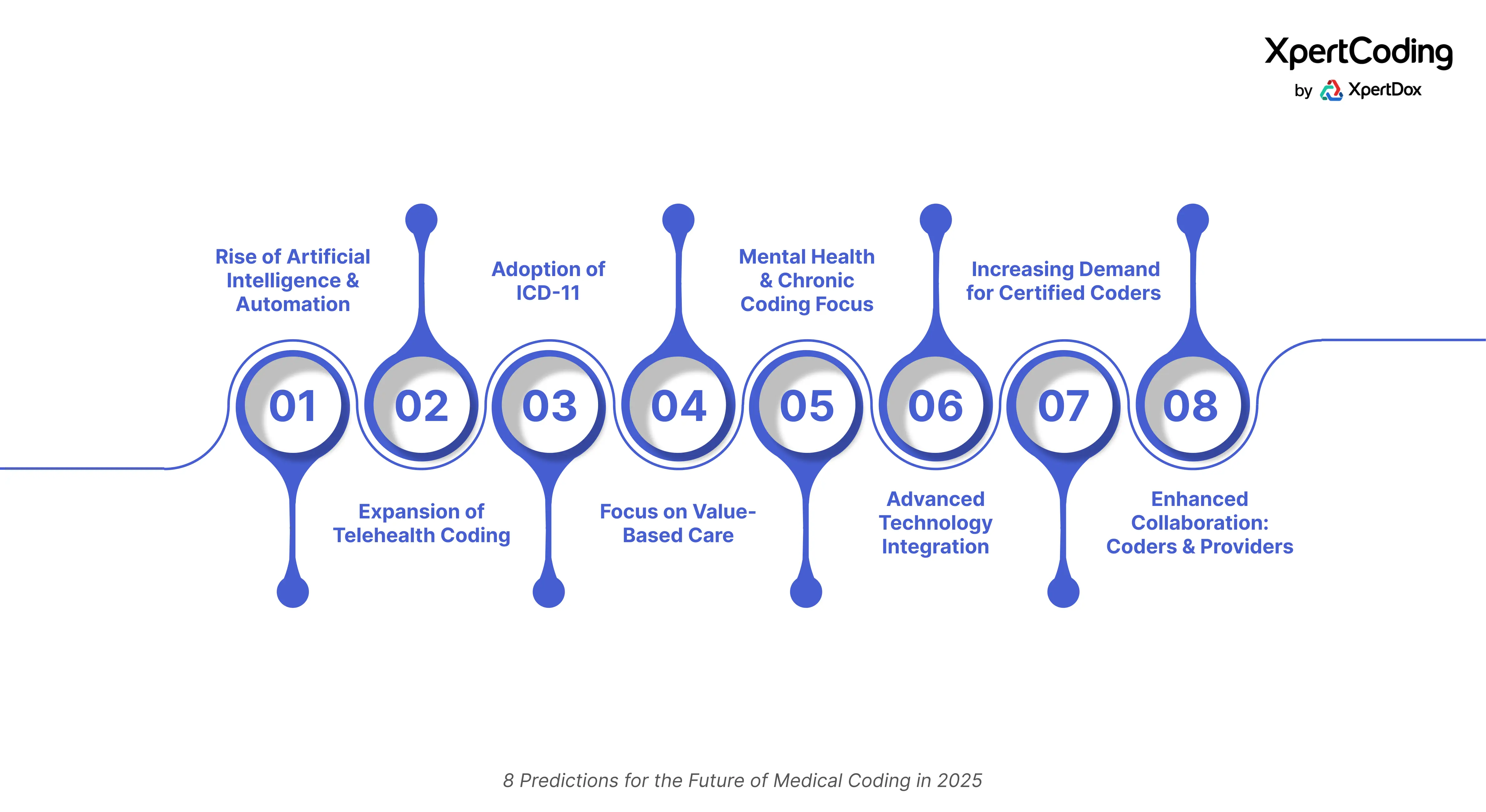
1. Rise of Artificial Intelligence and Automation
Artificial Intelligence (AI) and automation are already making significant strides in healthcare, and their impact on medical coding is set to grow exponentially by 2025. AI-powered systems can analyze clinical documentation, assign accurate codes, and even handle routine billing tasks with remarkable efficiency.
What to Expect by 2025:
- Sophisticated AI Systems: Advanced AI-driven coding software will process even the most complex cases, significantly reducing human error.
- Improved Efficiency: AI tools will handle high volumes of claims at unprecedented speeds, leading to fewer claim denials.
- Enhanced Decision Support: AI will act as a coding assistant, guiding human coders through complex cases while handling repetitive tasks.
While AI won’t replace human coders entirely, it will be an invaluable tool for improving accuracy and reducing workload, allowing coders to focus on strategic aspects of their work.
As AI becomes an invaluable tool for coders, exploring platforms like XpertDox’s AI-driven solutions can help coding professionals stay ahead.
2. Expansion of Telehealth Coding
The rapid adoption of telehealth during the COVID-19 pandemic has permanently altered the landscape of healthcare delivery. Telehealth services, ranging from virtual consultations to remote patient monitoring, are here to stay, and their coding requirements will expand accordingly.
What to Expect by 2025:
- New Telehealth-Specific Codes: More comprehensive codes will address diverse telemedicine services, including mental health consultations, chronic care management, and post-operative follow-ups.
- Stringent Guidelines: Payers will implement stricter scrutiny for telehealth claims, necessitating precise and up-to-date coding.
- Regulatory Updates: Governments and insurers will solidify policies for telehealth reimbursement, requiring coders to stay informed about evolving regulations.
Accurate telehealth coding will be critical to ensuring timely reimbursements, making it a focus area for coders and providers alike.
3. Adoption of ICD-11
The International Classification of Diseases (ICD) is a global standard for coding diseases and health conditions. By 2025, many countries will have adopted ICD-11, while U.S. continues to assess implementation timelines.
What to Expect by 2025:
- Enhanced Specificity: ICD-11 offers more granular detail, enabling coders to capture nuanced patient conditions.
- Global Standardization: The adoption of ICD-11 will facilitate better international comparisons of health data and outcomes.
- Training Needs: Coders will require extensive training to master the new system and ensure a smooth transition.
The shift to ICD-11 will revolutionize coding accuracy and interoperability but will also demand significant preparation from healthcare providers.
As ICD-11 becomes a global standard, leveraging tools like XpertDox's solutions may ease the transition by offering seamless updates and extensive training tools.
4. Focus on Value-Based Care
The healthcare industry is steadily shifting from volume-based care models to value-based care (VBC), where providers are rewarded for delivering high-quality outcomes rather than a high quantity of services.
What to Expect by 2025:
- Quality Reporting: Coders will play a crucial role in capturing patient outcomes and risk factors to support VBC programs.
- Bundled Payment Models: Accurate coding will be essential for documenting services provided during an episode of care under bundled payment arrangements.
- Compliance with New Standards: Coders must stay updated on guidelines for Medicare, Medicaid, and other VBC initiatives.
- Hierarchical Condition Categories: Coders will need to understand Hierarchical Condition Categories (HCC) to support accurate risk adjustment.
Value-based care will demand precise and comprehensive coding to ensure fair reimbursement and improved patient care quality.
5. Greater Emphasis on Mental Health and Chronic Disease Coding
As mental health awareness grows and chronic conditions become more prevalent, medical coding will need to evolve to address these areas effectively. Use of Z-codes for social determinants of health will grow as coding shifts towards capturing the full context of patient care.
What to Expect by 2025:
- Expanded Mental Health Codes: New codes will distinguish between mental health disorders by type and severity, improving care tracking and reimbursement accuracy.
- Detailed Chronic Disease Coding: Codes will reflect complications, co-morbidities, and long-term care needs more comprehensively.
- Integrated Behavioral Health Codes: As behavioral health and primary care integration increases, coding will reflect the full scope of services provided.
This evolution will ensure better resource allocation and care for patients with mental health and chronic conditions.
To accommodate the expanding domains of mental health and chronic disease management, innovative coding systems such as those provided by XpertDox could prove beneficial.
6. Integration with Advanced Technologies
By 2025, medical coding will become more integrated with cutting-edge technologies, including natural language processing (NLP) and blockchain.
What to Expect by 2025:
- NLP for Documentation: NLP tools will support real-time suggestions, helping coders select the most appropriate codes based on context.
- Blockchain for Data Security: Blockchain will enhance data transparency and security in coding and billing systems.
- Seamless EHR Integration: Coding systems will be tightly integrated with electronic health records (EHRs), ensuring real-time updates and accuracy.
These technologies will enhance the reliability and security of medical coding processes, improving trust and efficiency.
7. Increasing Demand for Certified Coders
As the complexity of medical coding grows, so will the demand for skilled and certified coders. By 2025, healthcare providers will prioritize hiring coders with specialized expertise and advanced certifications.
What to Expect by 2025:
- Specialization Opportunities: Coders will need expertise in niche areas such as telehealth, mental health, and value-based care.
- Continuous Learning: Continuing education will become essential as coding standards and technologies evolve.
- Certification Emphasis: Coders with credentials from organizations like AAPC and AHIMA will be in high demand.
Certified coders will be indispensable for navigating the changing landscape of medical coding and ensuring compliance with new standards.
Ensuring you have cutting-edge tools and continued education support like those found with XpertDox can make a significant difference in staying competitive.
8. Increased Collaboration Between Coders and Providers
Effective collaboration between coders and healthcare providers will become more critical in 2025. This partnership will ensure that documentation accurately reflects patient care and supports accurate coding.
What to Expect by 2025:
- Training for Providers: Healthcare providers will need training to improve documentation quality, making coders' jobs easier.
- Feedback Loops: Coders and providers will work closely to address documentation gaps and coding errors.
- Focus on Compliance: Collaborative efforts will help organizations stay compliant with changing regulations.
Strong collaboration will lead to more accurate coding, better reimbursements, and improved patient care.
Conclusion
As 2025 approaches, medical coding is poised for transformative changes fueled by advancements in technology, shifts in healthcare delivery, and evolving regulations. Key trends like AI integration, telehealth coding, value-based care, and ICD-11 adoption will enhance accuracy, efficiency, and adaptability. Certified coders, equipped with cutting-edge tools and knowledge, will play a critical role in ensuring seamless healthcare operations and financial stability.
By embracing these advancements and investing in training and technology, healthcare providers can navigate the challenges ahead, ensuring medical coding continues to be the backbone of effective healthcare delivery and a vital component of quality patient care.
Stay ahead of the curve with XpertDox’s AI-powered medical coding solutions. Their autonomous coding software, XpertCoding, accelerates claims submissions, ensures accuracy, and connects seamlessly with EHR systems. By reducing manual coding errors and delays, XpertCoding enhances financial performance, leading to faster collections and improved revenue. With a strong emphasis on security and compliance, XpertDox provides certified solutions to safeguard client information.
Contact XpertDox to transform your coding processes and secure your organization’s financial future.
Published on - 04/15/2025






